The Need for Pre-Authorizations Continues to Rise: Pros and Cons

Pre-authorizations, also known as prior authorizations (PA), have become a growing necessity in the healthcare industry.
Between 2009 and 2019, the use of prior authorization requirements in Medicare Advantage (MA) plans saw a significant increase across most service categories. More counties experienced over 90% exposure to prior authorization during this period. Today, approximately 75% of MA enrollees are in plans that mandate prior approval for certain services.
A 2023 survey by the Medical Society of the State of New York (MSSNY) revealed that most doctors have seen a big jump in the need for prior authorizations over the last five years. In particular, 71% of the physicians surveyed reported a significant increase in prior authorizations for prescription medications, and 64% noticed a similar rise for medical services.
Several factors drive the increased need for
prior authorization, including:
- The rising cost of healthcare
- The necessity for cost containment
- Compliance with regulatory changes and healthcare reforms
- Efforts to reduce fraud and abuse
- The increasing complexity of specialized healthcare services
- The shift towards value-based healthcare, ensuring patients receive medically necessary treatments
Many factors shape doctors' opinions on pre-authorizations, including their experiences with the process, the specific demands of different insurers, and their overall approach to patient care.
Improve prior authorization management with
billrMD!
Pros of Prior Authorization
Pre-authorizations are integral to the modern healthcare landscape, offering numerous benefits to care providers and insurers. Among the perceived advantages of prior authorization include:
1. Higher Quality of Care
Prior authorization helps ensure that doctors follow evidence-based medicine, which involves making healthcare decisions based on the integration of the best available research evidence, clinical expertise, and patient values and preferences.
Requiring doctors to justify their medical procedures and prescription choices with established guidelines and research promotes consistency and effectiveness in patient care. This process encourages the use of proven, safe, and effective treatments, ultimately improving the overall quality of healthcare.
2. Cost Control
One of the main advantages of insurance prior authorization is the role it plays in controlling healthcare costs. By requiring approval for specific medications, procedures, and treatments, insurance companies can ensure that healthcare facilities provide only the necessary and cost-effective options.
This step prevents the overuse of expensive treatments that may offer minimal benefits. Effective cost control through prior authorization can result in lower insurance premiums and out-of-pocket expenses for patients. Additionally, obtaining pre-authorization helps providers reduce the risk of non-payment or coverage disputes.
A
2023 research found that prior authorization reduces the use of preauthorized drugs by 25%, resulting in a 3% overall reduction in Medicare Part D spending. Notably, the savings from prior authorization are approximately ten times greater than the administrative costs required to implement it.
The reduction in Part D drug spending is approximately $95.88 per beneficiary per year, combining savings from restricted drugs and modest increases in spending on cheaper substitutes. This evidence demonstrates that prior authorization is a highly effective cost-saving measure.
3. Fraud Reduction
Prior authorization is essential for cutting down on fraud and abuse in healthcare. Insurance companies can spot and stop fraudulent claims by demanding thorough documentation and justification for treatments.
This oversight safeguards the healthcare system's integrity and ensures resources are used correctly. Reducing fraud and abuse saves money and supports the long-term sustainability of healthcare programs.
4. Patient Safety
Prior authorization helps prevent the overuse of certain medications and procedures, which can be potentially harmful to patients. By requiring pre-authorizations before the patient undergoes treatments, doctors and insurers can ensure that medications or procedures are truly necessary and beneficial. This extra layer of approval helps prevent patients from receiving redundant or inappropriate treatments, thereby reducing the risk of adverse effects.
5. Better Accountability in Healthcare
Requiring healthcare providers to justify their treatment decisions promotes accountability in the healthcare system. Prior authorization ensures that providers make informed and appropriate choices for their patients based on clinical evidence and best practices. Promoting accountability helps maintain high standards of care and fosters trust between patients, providers, and insurers.

Cons of Prior Authorization
While the intention behind prior authorization is to promote cost-efficient and safe patient care, its implementation often results in challenges for both patients and healthcare providers. Here are the perceived hindrances of insurance prior authorization.
1. Delays in Care
Prior authorization sometimes slows down critical patient care. Providers must navigate complex and varied insurance requirements or wait long for approval. A 2022 American Medical Association (AMA) survey found that 42% of healthcare providers indicated their patients frequently encounter delays in accessing care.
The AMA survey further disclosed that PA has led to hospitalizations, with 19% of respondents saying delays in insurance authorization have caused life-threatening events or necessitated interventions to avert them. Another 9% reported that PA delays have resulted in patients suffering from disabilities, congenital anomalies, permanent bodily damage, or death.
2. Increased Administrative Burnout
Prior authorization requires extensive documentation, back-and-forth calls with insurance companies, and constant follow-ups to secure approvals. The time healthcare staff spend on these tasks could be allocated to patient care. Moreover, this administrative burden overwhelms and burns out healthcare staff.
Based on the same 2023 AMA survey and
Annual Burden Report, 88–89% of physicians find the workload related to prior authorizations to be high or extremely high. About 35% have dedicated staff members who handle prior authorizations exclusively. On average, physicians complete 45 prior authorizations each week, which takes up nearly two full business days.
3. Interference with Clinical Judgment
Doctors frequently express concerns that pre-authorization protocols compromise their clinical autonomy and judgment. Some think these extensive requirements hinder their ability to determine the most suitable treatment plans, leading to significant frustration and feelings of constraint in delivering top-notch patient care.
4. Inconsistent Payer Policies
One frustrating aspect of prior authorization is the inconsistency in insurance policies. Different insurance companies have their own requirements and approval criteria. Because there's no standardization, what is approved by one insurer may be denied by another, causing inconsistent care and more administrative hassles.
5. High Administrative Costs
The administrative costs of getting pre-authorization can add up, diverting resources away from direct patient care and potentially increasing the overall cost of healthcare.
In 2019, processed
prior authorizations (PA) cost providers $528 million in administrative expenses. An AMA survey found that 86% of physicians believe
PAs lead to higher overall healthcare usage, causing unnecessary waste instead of saving costs.
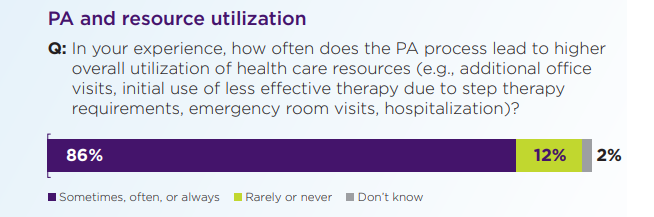
Source: 2022 AMA Prior Authorization Physician Survey
Ongoing Efforts to Improve Prior Authorization
Despite adding administrative strain and potential delays to the healthcare process, pre-authorization is essential in promoting cost-effective and evidence-based care. It helps prevent fraud and ensure the proper use of healthcare resources. The critical part is addressing the cons of prior authorization to allow doctors to deliver timely, high-quality patient care.
Expect to see a modernized healthcare system that eases the load on patients and providers through the government’s initiative to make a
more efficient prior authorization process. This development is part of the government’s ongoing efforts to boost health data exchange and ensure better access to care.
The Centers for Medicare & Medicaid Services (CMS) finalized this rule, which took effect on April 8, 2024. While the new policies are anticipated to save an estimated $15 billion over the next decade, the full impact is still being assessed.
Streamline Your Workflow with billrMD’s Insurance Verification
Doctors may have differing opinions on pre-authorization, but it remains an indispensable part of the healthcare system. Implementing strategies that optimize the process is crucial to enhance prior authorization management. By leveraging technology and innovative solutions, healthcare providers can better manage the pre-authorization process, ensuring timely and high-quality care for their patients.
billrMD’s medical billing system comes with an
Authorization and Referral Management module, which helps providers manage their workflow from a task management perspective. It allows quick identification of patients with upcoming appointments and highlights those whose authorizations are about to expire. Pre-authorization ensures that reimbursement is secured before the patient arrives for their appointment, streamlining the process and reducing administrative burdens.
Request a demo of billrMD or
try it for free to discover how our tools can help you manage prior authorization!
Recent Posts
One software for all your practice management needs.
billrMD | All Rights Reserved.
billrMD | All Rights Reserved.